A young woman sits in an examining room, waiting for her medical provider.
The provider arrives and picks up the chart. “I see you’re here to talk about family planning,” she observes. “What did you have in mind?” The young woman scans her memory: “What does my sister use? What about my friends? What have I seen on TV?”As we know from the work of psychologist and Nobel Prize winner Daniel Kahneman, author of Thinking, Fast and Slow, the preference she expresses is likely to be shaped by familiarity—whatever jumps to the front of her mind.
Now consider an alternative scenario: A young woman sits in an examining room, waiting for her medical provider. The provider arrives and picks up the chart. “I see that you’re here to talk about family planning,” he observes. “When do you think you might like to have your first baby?” As the conversation opens up, he follows with other questions: “What would you like to do before then? How big a deal would it be if you experienced an unexpected pregnancy? Ideally, how often would you like to get your period?”
In this scenario, the young woman finds herself having a very different conversation because rather than focusing on the surface question, a choice among contraceptive technologies, the provider has asked about what lies underneath: What is the young woman really after? What are her dreams and plans? How does this seemingly small, concrete decision about birth control relate to the life she wants to live?
Client Goals, Medical Expertise, Future Focus
Medical providers, allied health professionals, and reproductive health counselors are turning to a process called motivational interviewing to help young patients choose the birth control that best suits their lifestyle and goals. Motivational interviewing was first developed in substance abuse counseling. It recognizes that all of us, especially teens, have mixed feelings about taking care of ourselves and at times may be unsure of what we want. Rather than acting as an authority—“I know what’s best for you”—or taking a patient’s initial request at face value—“Whatever you say”—the provider using motivational interviewing opens up a collaborative process that respects both patient preferences and provider experience, leaving the final decision with the patient.
The field of reproductive health has a somewhat checkered history. When modern contraceptives first emerged, authoritarian, typically male doctors often adopted a “father knows best” attitude and sometimes strong-armed poor and minority females into using family planning methods they might not want. India’s early family planning incentives, China’s one-child enforcement, and American sterilization of minorities, criminals, and the mentally handicapped in the early 20th century are extreme examples of this paternalistic influence.
In reaction to practices like these, which we now understand to be violations of human rights, family planning initiatives shifted toward a model that simply responded to what women said they wanted. This solved some of the worst reproductive justice problems but caused others, because young and underprivileged women are less likely to have access to information that would enable them to make the best decisions to meet their objectives, and they may not have the health literacy or efficacy to make their preferences apparent during a brief health care encounter.
This model also violated what we know to be excellent medical practice. If a teen sees her primary care provider for athlete’s foot, the provider doesn’t ask, “What medication do you want?” Rather, the teen trusts the provider to help diagnose her situation and then recommend the most effective treatment that is safe and appropriate. That is the provider’s responsibility.
In reproductive health, motivational interviewing is used to help develop what is known as a reproductive life plan—a tentative and flexible outline that weaves questions about whether, when, and how to have children into a broader fabric of personal goals. This doesn’t have to be as daunting as it sounds. Oregon has launched a program, One Key Question, aimed at getting primary care providers to ask, at every visit with women, “Would you like to become pregnant in the next year?” The goal is to have births be “wanted, planned, and as healthy as possible.”
Choice Architecture

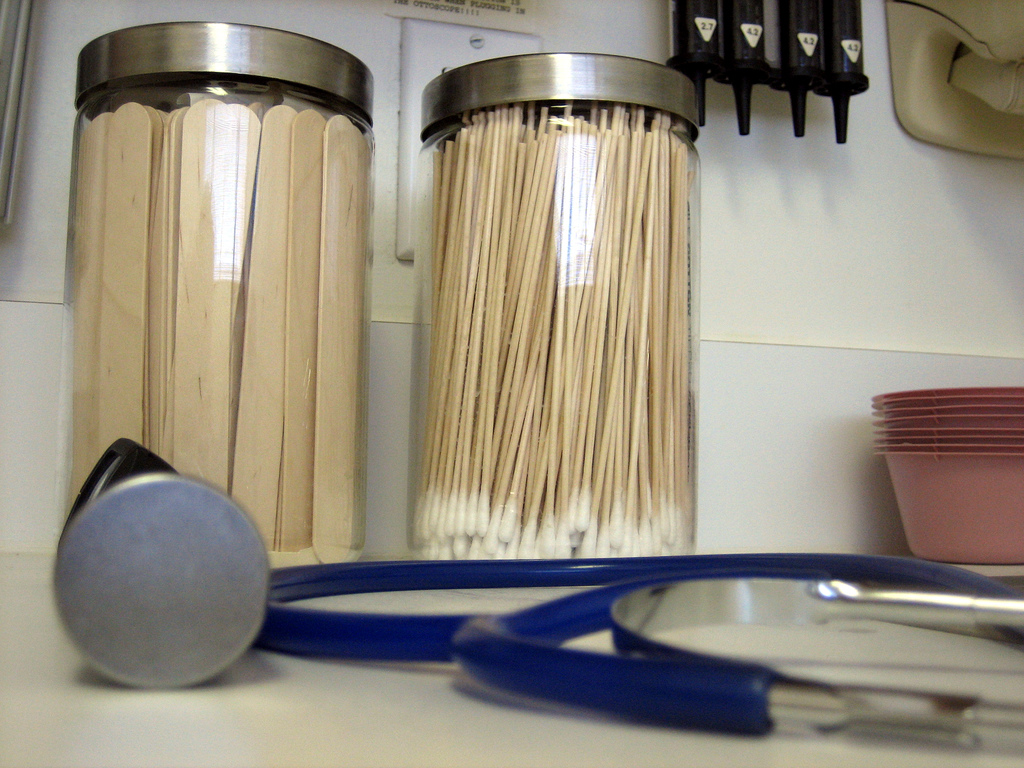
Nursing by Christiana Care used under CC BY-NC-SA 2.0
Along with the move toward patient-centered counseling techniques such as motivational interviewing, medical providers are making a second shift in how they talk about contraceptive options. In the past, providers often started by talking about the most familiar methods first, namely the pill, condom, or other self-administered methods. But we now know that the sequence and presentation of information influences the decisions people make. Behavioral economists call this sequencing choice architecture. For example, when public schools switched to putting apples in front of cookies on school lunch lines, more students chose apples.
Similarly, when researchers in St. Louis offered 9,000 women the contraceptive of their choice, they presented the options in order of efficacy, and almost 75 percent of the women chose a top-tier long-acting reversible contraceptive (an IUD or implant), with dramatic improvements in health outcomes. Even a majority of teen participants opted for an IUD or implant, contradicting the oft-cited beliefs among providers that teens either are not interested in or are not appropriate candidates for long-acting contraceptives. Such methods are 20 times more effective than the pill, so rates of teen pregnancy and abortion plummeted, and more women said they were pleased with their contraceptive choice.
After seeing the promising results of the St. Louis approach, family planning providers are switching to a “tiered” presentation of birth control options. When a woman communicates that her first priority for a method is pregnancy prevention, they start at the top of the list in terms of efficacy (the top tier) and work their way down till they find a method that fits her lifestyle preferences and health conditions. The World Health Organization and CDC and public health advocates such as the National Campaign to Prevent Teen and Unintended Pregnancy and the California Family Health Council have also started structuring information to increase visibility of the most effective methods.
Preconception Health Care
Public health officials are more focused than ever on promoting planned pregnancy for an important reason. New research suggests that what a woman ingests during the first weeks of pregnancy and in the weeks before conception has an effect on fetal development. Certain nutrients, including B vitamins, choline, and folic acid, appear to trigger epigenetic effects, meaning they influence how genes in the DNA sequence get expressed. As this information has emerged, the Centers for Disease Control has amped up outreach about “preconception health care.” In addition to the folic acid supplementation that is a current standard of preconception health care, providers may also start providing guidance on additional nutrient requirements for women to promote healthy conception and pregnancies. And of course, preconception health care requires planned childbearing.
Better Listening, Better Tools
For many years, data have been accumulating that show a link between well-timed childbearing and family well-being, including financial stability, education, and maternal and child health. Despite that evidence and the availability of safe and effective contraceptive methods, close to half of the pregnancies in the United States are unplanned. For teens, that number rises to over 80 percent. Many of these pregnancies result in unexpected but welcome and well-supported childbearing. Even so, it is becoming increasingly clear that if we want to give children the best possible opportunity for a healthy and productive life, we need to give youth and women the knowledge and tools to time their pregnancies.
New contraceptive tools such as state-of-the-art IUDs and implants are total game-changers when it comes to empowering planned pregnancy and reducing “accidents,” and some people worry that enthusiasm in the public health community could mean that once again women may get pressured to use methods they don’t want. That is why tiered presentation of contraceptive options needs to be tied to patient-centered counseling techniques designed within a human rights–based framework. When a family planning provider takes the time to elicit a patient’s objectives and to help her create a “reproductive life plan,” then the provider can bring to bear expertise about contraceptive options and healthy gestation, confident that he or she is serving the patient’s own interests.
Knowing what the patient’s goals are, how willing she is to experience an unexpected and unplanned pregnancy, what procedures or side effects she is most accepting of, and how she would like to manage her menstrual cycles. All of this allows the provider to make a knowledgeable recommendation of the most effective method(s) that will meet the patient’s goals.